If you are living with senior citizens in your home, you may observe that their bedtime is much, much earlier—unlike younger people, fond of staying awake until late at night with little difficulty—although they are also the first to get up in the morning without any alarms to wake them. These sleep behaviors are the most common changes observed among the elderly. What exactly changes within us when we age that affects our sleep? What changes can we expect once we reach the golden years? Let’s take a closer look what studies have discovered so far, so that we can understand these changes a little more.

What Are the Stages of Sleep?
Before we look into the changes that aging brings to sleep, let’s have a quick view on the different stages of sleep that we go through on an average night. There are five stages of sleep currently known:
Stage One: The start of the process- this is where we get ourselves to a comfortable position and prepare to drift off. Our brain generates alpha and theta waves, where we exhibit relaxation and drowsiness. People exhibiting alpha waves usually experience strange yet vivid sensations, sometimes a feeling of falling which is followed by sudden muscle contractions- the leg jerk that we feel when we are almost asleep. Meanwhile, as we enter the theta state, we alternate between wakefulness and sleep, which usually takes several minutes.
Stage Two: Our brain produces sleep spindles, which are minute periods of rapid and rhythmic brain wave activity. This is also where our body temperature lowers, together with a decreasing heart rate.
Stage Three: Next, our brain begins to emit delta waves, which result to a deep and dreamless sleep. Brainwave frequency in this stage is very low, around 1.5 to 4 cycles per second. We also transition between light and deep sleep during this period.
Stage Four: This is where we experience deep sleep, and where delta waves are most prominent- sleep disorders, like sleepwalking and nocturnal incontinence usually happen in this stage. It lasts more or less about 30 minutes.
Stage Five: Also known as the Rapid Eye Movement (REM), is also the last stage of sleep before the process cycles back to stage two and repeats all through the night. This stage is characterized by eye movement (hence the name), and increase in respiration and brain activity, which would explain why dreams occur in this period. Despite the active neurological activity, voluntary muscle movement is restricted, and you can’t run or jump while you are asleep under normal circumstances.
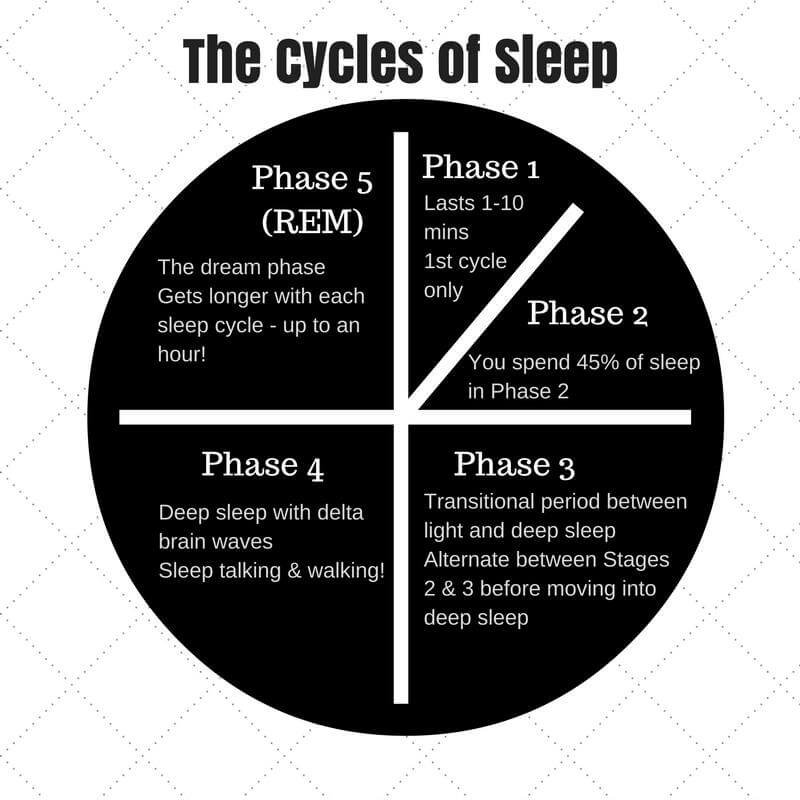
The cycle isn’t a perfect circle: once we complete stage one to four, we then go back to stage two and three a couple more times until we reach stage four and finally achieve REM sleep, which is around 90 minutes after we start the process. The cycle becomes longer and longer with each turn, and REM can even last for an hour as our sleep progresses.
Decreasing Sleep with Increasing Age
This study compiled different literature relating to changes in sleep due to aging, and found that we lose 10 minutes of sleep per decade, with those above 60 years old experiencing a decrease of 2% in stage 3 sleep per decade. Meanwhile, a more subtle decline is observed in REM sleep. These changes then result to increased periods of stage one and two, resulting to more frequent arousal and awakening.

Declining Growth Hormone Levels
Meanwhile, this study presents an interesting relationship between the decline in deep sleep among elderly individuals and growth hormone (GH) levels, specifically for men. This hormone is primarily responsible for growth in children and adults, with some functions in body composition and fluid regulation, muscle and bone growth, and metabolism. Researchers discovered that the decline in deep slow wave sleep from early adulthood (16 to 25 years old) to midlife (36 to 50 years old) paralleled with a significant decline in growth hormone secretion (up to 75%), while the decrease becomes slower from midlife to old age.
They also observed sleep duration decreasing with age, with significant reductions happening later in life. They estimated that from midlife to the 80s, the total sleep time is reduced by an average of 27 minutes per decade. Moreover, decrease in REM sleep and wake time increase were not apparent until the fifth decade, where increase in cortisol levels were also observed. Cortisol is called the “stress hormone” because of its association with stress responses, while also regulating a variety of processes like blood sugar levels, metabolism, memory formation, and salt and water balance. It’s concluded that sleep quality changes from midlife to old age are associated with alterations in hormonal secretions.
Weaker Regulation of Circadian Rhythms
Another human function that changes as we age is our circadian rhythm. For the uninitiated, it is our internal body clock that regulates our sleep and wake cycles. While the hypothalamus has the primary responsibility of controlling the circadian rhythm, outside factors also affect its regulation, like light exposure, posture, sleep schedule, and food intake.

This literature compiles the different studies about circadian rhythm and its changes with aging, and found that reduced amplitude of output signals from the circadian rhythm is observed among the elderly. This suggests that sleep changes relative to aging may be due to weaker circadian regulation of the sleep/wake cycle. It is not yet known which part of the cycle is affected by this- sleep or wakefulness, although a nap study suggests that circadian wake signals were weaker in older people, which is maybe why they tend to take more mid-day naps, which result to less consolidated and shorter sleep during the night.
Gender Disparity in Sleep Changes
Another interesting discovery that the above mentioned study showed is that men are more affected by women when it comes to these changes- they have a decrease in total sleep hours, decreased percentage of stage 3 and REM sleep, and increased percentage in stage 2 sleep, as well as increased frequency of waking up in the middle of their slumber as compared to women. What’s more interesting though is that women reported shorter and poorer sleep compared to men, which could explain why they use sleeping medications more frequently.

This does not necessarily mean that women’s reports of sleeping difficulties are inaccurate, especially since menopause does have an effect on sleep. Estrogen, the primary sex hormone in women, assists in promoting healthy sleep by helping the body absorb and utilize serotonin and other sleep-inducing neurochemicals. Menopause causes estrogen levels to dive below the usual, until production is put to a complete stop, and quality sleep is therefore less achieved- in fact, insomnia is one of the earliest signs of this period.
The Bottom Line
Now that we understand how and why sleep changes as we age, it may be a good idea to get some quality zzz’s while we are still in our prime, and more importantly, while we still can. Knowing that sleep will become less both in quality and quantity as we grow older, it’s important that we sleep soundly and comfortably while we are not yet experiencing these changes. If you’re already having some difficulty on this right now, a proper mattress, certain sleeping accessories, and sleeping aids may help.